Your horse just isn’t quite right. His performance has been a little off lately, you’ve noticed him stumbling now and then, and he seems to be losing muscle over his topline. He’s not actually lame. So what’s going on?
With symptoms like those, there’s a good chance your horse might be facing a neurological disorder. Many things—including trauma, degenerative conditions, viruses and parasites—can disrupt the signals flowing along your horse’s spinal cord from the brain to the nerves and muscles.
“Detecting symptoms early increases the likelihood of successful treatment and recovery,” says the University of Pennsylvania New Bolton Center’s assistant professor Amy L. Johnson, DVM, DACVIM in both internal medicine and neurology. That’s because neurological disorders affect neurons (nerve cells), and “once neurons are destroyed, they don’t regenerate,” says Dr. Johnson.
If a neurologic disorder is left untreated, she adds, more neurons become affected and more of them die. “Horses can compensate for losing some neurons, but once a critical number are lost, normal function will never return. And almost all neurological diseases can be fatal, depending on the severity and whether or not treatment is provided.”
That’s why it’s critical for horse owners to know the signs of potential neurologic trouble and act quickly to bring a vet onto the scene. Here, Dr. Johnson shares red flags to watch for, plus an inside perspective on what your vet will do to pinpoint the trouble and put your horse on the road to recovery.

Signs to Watch For
“The most common indication of a neurologic problem in horses is some degree of clumsiness or incoordination,” says Dr. Johnson. That’s because neurologic disorders often affect the spinal cord, which delivers messages to all of the horse’s limbs. So you might notice your horse standing in unusual positions—say, with his legs crossed or placed more widely than usual. Or your horse might trip, stumble, move more slowly than normal or have trouble performing his regular work.
Other neurological disorders affect the brain. If the front brain is involved, you may spot alterations in your horse’s behavior and mental status, says Dr. Johnson. For instance, she adds, “If your 3-year-old Thoroughbred is acting like a 20-year-old pony, that could be an indication of trouble.” Other signs of a front-brain problem include obsessive circling, aimless wandering and staggering.

“If the problem is in the back part of the brain, or the brain stem, the horse may have an unusual appearance to his face, similar to a person who has suffered a stroke,” says Dr. Johnson. “You may see drooping of an ear or eyelid, the nose pulled to one side, a tilt to the head. The horse may have trouble eating or drinking, even to the point where food is coming out the nose.”
Other general signs of potential neurological trouble include muscle loss, often on one or both hips, or over the topline. Your horse may not swish his tail or twitch his skin like he normally does—for example, to keep flies off. You may see an overall drop in condition or your horse may suddenly have trouble maintaining weight or may lose his appetite. Certain disorders could contribute to neck pain, leading your horse to resist bending his neck or raising/lowering his head, or causing a loss of suppleness.
If you notice any of these signs, it’s time to call the vet.
What to Expect from Your Vet
When your vet arrives on site, expect her to start with a basic physical exam, taking your horse’s heart rate, respiratory rate and temperature and checking for gut sounds. At this stage, the vet is looking to eliminate the possibility of a systemic (body-wide) disease, such as septicemia (bacteria or toxins in the bloodstream) or equine infectious anemia. says Dr. Johnson, because “most neurological disorders don’t cause systemic problems, but systemic disease can occasionally make a horse look neurologic.”
Your vet will also ask you to discuss the symptoms you’ve seen, including changes in your horse’s personality, such as lethargy or aggression. Share as much detail as you can on the circumstances, such as when the signs started and how often they occur. Your horse’s age and breed may also play a role, since some neurological problems tend to be more common in certain groups.
Your vet will also take in the big picture, looking your horse over for any signs of asymmetry in posture or muscling, muscle atrophy or lack of condition.
Your vet will then begin conducting specific tests to pinpoint whether your horse’s problems are related to a neurological disorder and, if so, which part of the nervous system is most likely the source of trouble. These tests typically include procedures to check facial reflexes, body reflexes and your horse’s gaits and posture.

Facial Reflexes
“There are 12 cranial nerves that influence the horse’s ability to see, chew, swallow and have symmetrical expressions, among other things,” says Dr. Johnson. To test how well these nerves are doing their job, she notes, your vet may conduct any of a number of tests on both sides of the horse (where applicable). Here are a few examples:
- Testing your horse’s “menace response.” The vet moves her hand quickly toward the horse’s eye to see whether he blinks. This tests the horse’s ability to see and to close his eyelids.
- Checking for skin sensation. The vet taps along the side of the horse’s face, from the ear to the nostril. The horse should blink and/or attempt to move away from the tapping.
- Testing the ability to chew and swallow. The vet may give the horse a treat or watch the horse eat and drink.
- Testing tongue strength and function. The vet gently pulls the horse’s tongue out through the bars on one side of the mouth and then watches to see if the horse can pull it back in.

Body Reflexes
Again, the vet may perform any or all of the following tests on both sides of your horse to check for normal responses. Typically, a lack of reaction to any test or in a specific area indicates that nerve signals may not be reaching that location.
- Neck range of motion. The vet may encourage your horse to bend his neck to each side, stretching toward the hip, stifle or hock, or down between the front legs, often using a carrot or other treat as an incentive. If your horse has trouble with this exercise, it could indicate an injury to his neck, such as a fractured vertebra or neck arthritis. Other indications of neck trouble include difficulty raising the head, holding the head or neck in an unusual position, loss of suppleness through the neck and reluctance to bend during work.
- Skin sensation. Your vet will lightly run or tap a pen along your horse’s skin to watch for a twitching response—the reaction your horse would have to a fly landing on his skin.
- Reaction to pressure. Your vet will palpate your horse’s topline, neck, chest, hindquarters and stifles to see if he moves away from the pressure or otherwise reacts.
- Tail tone and body strength/coordination. A horse’s tail receives nerve signals from the spinal cord, so your vet will also conduct tests to make sure those messages are getting delivered. For instance, she may lift the tail to check for resistance; if the tail is limp, that’s a sign of trouble. To test your horse’s body strength and coordination, she may also pull the tail gently to each side while your horse is standing and/or walking. If the pull shifts your horse off balance, that’s another red flag.

Gait and Posture Assessment
In the next stage of a neurological evaluation, your vet will assess your horse’s gaits and posture. In general, these tests will show whether the horse knows where his feet are and has normal control over his limbs.
Your vet may ask you to walk your horse on varying surfaces, up or down a slope and a curb or step, in a tight circle in each direction and to back up. She may want to see your horse moving freely in a round pen as well as moving in hand. She’ll watch to see if your horse stumbles, sways, staggers, drags his toes, swings a hind leg, steps on himself or shows other signs of incoordination or gait abnormalities.
Your vet may also pick up one of your horse’s feet and place it so it crosses in front of its opposite. For example, she may lift the left front and place it over the right front. A horse with a neurological problem may leave the foot out of place for a while before moving it back into position.
Going to the Next Level
By this point in the exam, your vet will probably have a strong sense of whether your horse has a neurological problem, says Dr. Johnson. If the issue doesn’t seem neurologic, she adds, the vet will carry on looking for other possible causes for what you’re seeing, such as conducting a lameness exam or oral exam because problems with chewing and swallowing, for instance, can be caused by dental troubles.
If your vet decides there is a neurologic disorder, the next challenge is determining the underlying cause. It’s not as simple as you might think. “The actual neurologic signs the horse shows depend almost entirely on what part of the nervous system is affected, rather than the disease itself,” says Dr. Johnson. “In other words, the neurologic signs of brain injury can be similar regardless of whether the brain is injured due to trauma, abnormal liver function or infection such as equine protozoal myeloencephalitis. However, other signs might help identify the underlying cause.”
Following are several examples of common neurological disorders and the symptoms and diagnostic aids that can help your vet distinguish one from another.

Trauma
If your horse has experienced an injury to the skull or any part of the spine—for instance, from hitting his head or falling—that’s a strong indication that trauma could be the trouble. Symptoms of a problem could be immediate, such as unconsciousness, disorientation or temporary blindness. Or they may not appear for a while and then could include trouble getting up or lack of coordination.
Diagnostics: Radiographs (X-rays) to check for possible fractures of the skull or spinal vertebrae.
Equine Protozoal Myeloencephalitis
Loss of coordination is one of the most common symptoms of EPM along with muscle atrophy affecting only one side of the horse, says Dr. Johnson. EPM horses may also show signs of back brainstem impairment, such as partial facial paralysis and trouble swallowing.
Diagnostics: Blood and spinal-fluid tests to look for antibodies to the EPM-causing parasite. Both tests are recommended because in areas where EPM is prevalent, it’s not uncommon for 50 percent or more of the equine population to have antibodies to the disease. That could cause a positive blood test even if a horse isn’t infected, explains Dr. Johnson. If the antibodies are also present in spinal fluid at an increased level compared to blood, that provides a much more accurate diagnosis, she says.
Equine Herpesvirus-1
EHV-1 is more commonly seen in outbreaks involving a number of individuals, says Dr. Johnson. So if multiple horses in an area start exhibiting similar symptoms, that’s an indication this disease could be the culprit. Affected horses may run a fever and lose control over when they urinate or pass manure (urinary and/or fecal incontinence). They may show weakness in their tail muscles. The back legs are more often affected, which can lead to the horse having trouble rising and, instead, taking on a “sitting dog” position partway up.
Diagnostics: Polymerase chain-reaction tests to identify the virus in blood samples or nasal swabs. (A PCR test allows the vet to analyze viral DNA even when very small amounts are present in a sample.)
Wobbler Syndrome
Officially known as cervical vertebral stenotic myelopathy or cervical vertebral malformation, “wobblers is a problem with the vertebral column in the region of the neck,” says Dr. Johnson. Specifically, abnormal vertebrae cause compression on the spinal cord, which can block nerve signals.
“Symptoms tend to be in all four limbs, although they may be more evident in the back legs,” says Dr. Johnson. She adds that the disease can look a lot like EPM, but wobbler horses might have neck pain while EPM horses won’t.
Diagnostics: Blood and spinal-fluid tests to rule out EPM, radiographs to eliminate a vertebral fracture and show vertebral changes suggestive of wobbler syndrome and/or a myelogram (see sidebar on page 55) to identify pressure on the spinal cord.
Eastern and Western Equine Encephalomyelitis, West Nile Virus
These mosquito-borne diseases all affect the horse’s spinal cord and brain, says Dr. Johnson. “They have symptoms indicative of brain problems—weird behavior, they may lose the ability to stand up, they may have fevers,” she adds. The horse may also exhibit head-pressing (literally, the horse presses his head against a surface such as a stall wall) and aimless wandering, lose his appetite, appear depressed, have impaired vision or show muscle twitching and hind-limb weakness. Dr. Johnson notes that horses with West Nile virus may present with more spinal symptoms than EEE or WEE horses but almost always have brain signs as well.
Diagnostics: Blood and spinal-fluid tests are taken by your veterinarian.
Next Steps
Since it may take days to get results from diagnostic tests (and even then more advanced testing may be needed), your vet may start your horse on an initial treatment plan immediately. This might include therapies directly aimed at the suspected disorder (see sidebar on page 56). Or it may focus on supportive treatments—such as intravenous fluids or anti-inflammatories—to keep your horse comfortable and as stable as possible until a final diagnosis is made.
This inherent delay in the process is just one more reason it’s important for you to know the symptoms of neurological trouble. Then you can start the ball rolling quickly on a diagnosis so treatments can begin and your horse can start his journey to recovery.

Common Neurological Disorders Defined
Disorders of the horse’s central nervous system fall into multiple categories. These include (but aren’t limited to) degenerative, nutritional, metabolic, immune-mediated, toxic and infectious. “In adult horses, the most common categories would be degenerative [arthritis], anatomic and infectious,” says Dr. Johnson. The latter category includes viral, bacterial and parasitic causes, she adds.
Here’s an overview of the causes, preventions and treatments for the diseases discussed.
Equine Protozoal Myeloencephalitis
Cause: Horses become infected by consuming food or water contaminated with opossum feces containing the parasite Sarcocystis neurona, which then moves into the horse’s central nervous system. Horses under 5 and over 13 may be at higher risk. Anything that compromises your horse’s immune system can also increase risk.
Prevention: Minimize your horse’s exposure to opossum feces. In areas with opossum populations, avoid feeding your horse off the ground and keep feed stored away safely.
Treatment: There are three FDA-approved medications to fight S. neurona—ponazuril, diclazuril and sulfadiazine used in combination with pyrimethamine. Some vets may also recommend a vitamin E supplement.
Eastern and Western Equine Encephalomyelitis and West Nile Virus
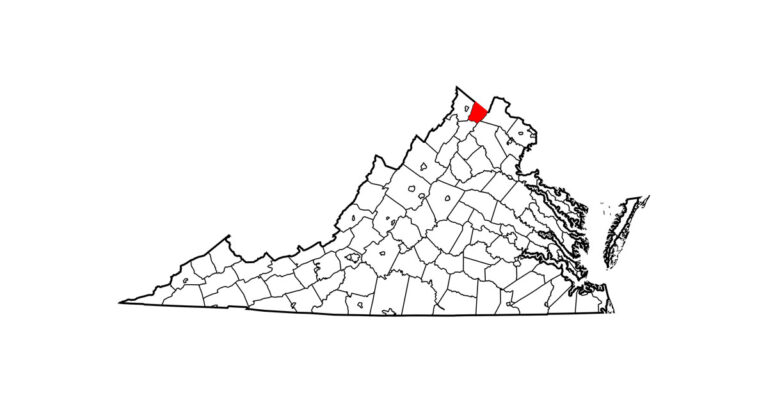
Cause: These viral diseases are spread by infected mosquitoes with the virus attacking the horse’s central nervous system. WEE is seen in western North America and as far south as Argentina. EEE has appeared in every U.S. state east of the Mississippi as well as a few other states. West Nile virus is prevalent over the entire U.S.
Prevention: Vaccinate your horse as recommended by your veterinarian and practice good mosquito mitigation.
Treatment: There is no treatment for these diseases. Your vet can provide supportive therapy—for instance, treating a fever, providing intravenous fluids and nutrition and treating any secondary infections.
Equine Herpesvirus-1
Cause: This viral disease is spread by direct horse-to-horse contact or with a contaminated object, such as buckets, clothing or skin that have been in contact with an infected horse. While many horses are exposed to the disease early in life, the virus can be inactive for years and appear during times of stress, like long-distance transport or strenuous exercise.
Prevention: Vaccinate. “The vaccination does not protect the horse from the neurologic form of the disease,” says Dr. Johnson. “However, it might help reduce viral spread during an outbreak, leading to fewer affected horses.” Be cautious of allowing your horse to have contact with other horses or communal water troughs at shows and other places where horses from different locations gather.
Treatment: Supportive care. Antiviral drugs might help prevent disease or limit its effects, says Dr. Johnson. Treatment for secondary concerns might also be warranted, such as anti-inflammatories or antibiotics.
Wobbler Syndrome (Also known as cervical vertebral stenotic myelopathy or cervical vertebral malformation)
Causes: Wobblers affects the horse’s neck and may be caused by bone malformation, malarticulation, developmental bone disease or arthritis. The common result is that the vertebrae press against the spinal cord, causing compression that can interfere with nerve messages traveling from the brain to the limbs.
Prevention: None. “Breeding horses known to have wobblers is not recommended,” notes Dr. Johnson. “Pushing young horses for rapid growth might contribute to disease in genetically predisposed individuals.”
Treatment: Depending on the cause, treatment includes surgery, anti-inflammatory medication, physiotherapy, stall rest or nutritional changes.

Diagnostic Aids for Neurological Cases
Diagnostic tools, like those below, are essential to helping your vet get the most accurate picture of the cause behind a horse’s neurological problem. While the first three tests are relatively common, in some cases your veterinarian may want to use the other tools to provide more clarity or detail to provide a more precise diagnosis.
- Blood tests to check for antibodies to specific equine diseases
- A spinal tap to check for antibodies or evidence of inflammation of the nervous system; Dr. Johnson, an assistant professor at the University of Pennsylvania New Bolton Center, further explains that “certain patterns of inflammation can give the vet a hint as to the type of disease, showing evidence of parasites, fungal infection or tumors.”
- Radiographs (X-rays) of the neck or spine to check for signs of wobblers, arthritic changes or fractures
- Myelograms, which are a special type of radiograph where your horse is anesthetized and laid down on his side, a contrast agent (dye) is injected around his spinal cord and images are taken with your horse’s neck in different positions. They can accurately identify pressure on the spinal cord or vertebral narrowing or instability, confirming what may only be suspected from an X-ray.
- Magnetic resonance imaging, a diagnostic imagining technology that could allow a veterinarian to identify structural problems or inflammation of the brain or spinal cord
- Computed tomographyscans, which provide high-resolution images of bone and some soft-tissue structures in multiple planes, yielding much more information than standard radiographs
- Electrodiagnostic testing to assess nerve and muscle function, although Dr. Johnson notes that this is not a common diagnostic tool because it requires specialized expertise and equipment only available through a limited number of veterinary hospitals
- Nuclear scintigraphy, also known as bone scans, can show inflammation in the bones or where ligaments attach to bone.
Dr. Johnson notes that diagnostics are one area of equine neurology that’s seen improvements in recent years. For instance, “the knowledge of needing to compare blood and spinal fluid [to identify EPM] is really recent,” she notes. In addition, she says, “Imaging is getting better. We’re able to image more parts of the horse. We do more brain MRIs in horses than in the past. We can take CT scans of the horse’s neck and, here at the University of Pennsylvania, we now have a robotic CT system” that allows vets to scan more of the horse more easily. (For an overview of the robotic CT scanner, check out the article here)
This article was originally published in the December 2017 issue of Practical Horseman.